extract from The Wall Street Journal, By Daniela Hernandez, Sarah Toy, and Betsy McKay,
How Exactly Do You Catch Covid-19? There Is a Growing Consensus
Surface contamination and fleeting encounters are less of a worry than close-up, person-to-person interactions for extended periods
Six months into the coronavirus crisis, there’s a growing consensus about a central question: How do people become infected?
It’s not common to contract Covid-19 from a contaminated surface, scientists say. And fleeting encounters with people outdoors are unlikely to spread the coronavirus.
Instead, the major culprit is close-up, person-to-person interactions for extended periods. Crowded events, poorly ventilated areas and places where people are talking loudly—or singing, in one famous case—maximize the risk.
These emerging findings are helping businesses and governments devise reopening strategies to protect public health while getting economies going again. That includes tactics like installing plexiglass barriers, requiring people to wear masks in stores and other venues, using good ventilation systems and keeping windows open when possible.
Two recent large studies showed that wide-scale lockdowns—stay-at-home orders, bans on large gatherings and business closures—prevented millions of infections and deaths around the world. Now, with more knowledge in hand, cities and states can deploy targeted interventions to keep the virus from taking off again, scientists and public-health experts said.
That means better protections for nursing-home residents and multigenerational families living in crowded conditions, they said. It also means stressing physical distancing and masks, and reducing the number of gatherings in enclosed spaces.
“We should not be thinking of a lockdown, but of ways to increase physical distance,” said Tom Frieden, chief executive of Resolve to Save Lives, a nonprofit public-health initiative. “This can include allowing outside activities, allowing walking or cycling to an office with people all physically distant, curbside pickup from stores, and other innovative methods that can facilitate resumption of economic activity without a rekindling of the outbreak.”
The group’s reopening recommendations include widespread testing, contact tracing and isolation of people who are infected or exposed.
Getting the Covid-19 virus involves three steps.

1 Coughing, talking and breathing creates virus-carrying droplets of various sizes.
2 Enough virus has to make itself over to you or build up around you over time to trigger an infection.
3 The virus has to make its way into your respiratory tract and use the ACE-2 receptors there to enter cells and replicate.
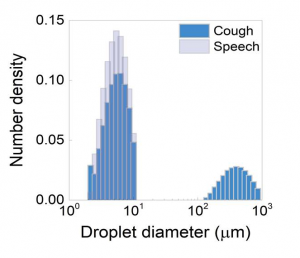
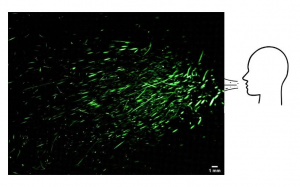
One important factor in transmission is that seemingly benign activities like speaking and breathing produce respiratory bits of varying sizes that can disperse along air currents and potentially infect people nearby.
Health agencies have so far identified respiratory-droplet contact as the major mode of Covid-19 transmission. These large fluid droplets can transfer virus from one person to another if they land on the eyes, nose or mouth. But they tend to fall to the ground or on other surfaces pretty quickly.
Some researchers say the new coronavirus can also be transmitted through aerosols, or minuscule droplets that float in the air longer than large droplets. These aerosols can be directly inhaled.
That’s what may have happened at a restaurant in Guangzhou, China, where an infected diner who was not yet ill transmitted the virus to five others sitting at adjacent tables. Ventilation in the space was poor, with exhaust fans turned off, according to one study looking at conditions in the restaurant.
Aerosolized virus from the patient’s breathing or speaking could have built up in the air over time and strong airflow from an air-conditioning unit on the wall may have helped recirculate the particles in the air, according to authors of the study, which hasn’t yet been peer-reviewed.
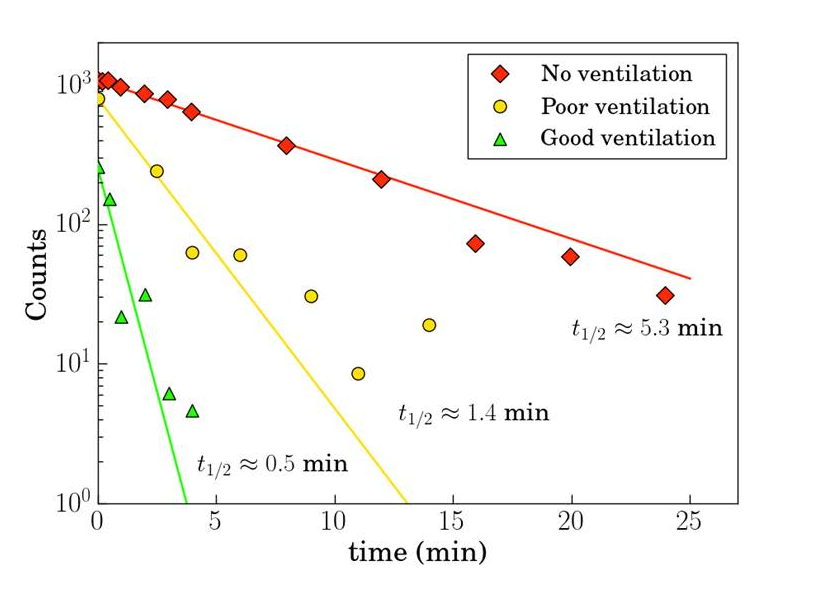
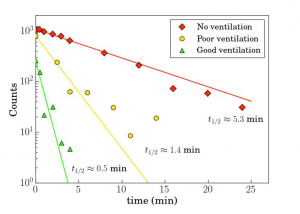
Sufficient ventilation in the places people visit and work is very important, said Yuguo Li, one of the authors and an engineering professor at the University of Hong Kong. Proper ventilation—such as forcing air toward the ceiling and pumping it outside, or bringing fresh air into a room—dilutes the amount of virus in a space, lowering the risk of infection.

A gym in Chino Hills, Calif., on June 12. PHOTO: WILL LESTER/ORANGE COUNTY REGISTER/ZUMA PRESS
Another factor is prolonged exposure. That’s generally defined as 15 minutes or more of unprotected contact with someone less than 6 feet away, said John Brooks, the Centers for Disease Control and Prevention’s chief medical officer for the Covid-19 response. But that is only a rule of thumb, he cautioned. It could take much less time with a sneeze in the face or other intimate contact where a lot of respiratory droplets are emitted, he said.
Superspreaders
At a March 10 church choir practice in Washington state, 87% of attendees were infected, said Lea Hamner, an epidemiologist with the Skagit County public-health department and lead author of a study on an investigation that warned about the potential for “superspreader” events, in which one or a small number of people infect many others.
Members of the choir changed places four times during the 2½-hour practice, were tightly packed in a confined space and were mostly older and therefore more vulnerable to illness, she said. All told, 53 of 61 attendees at the practice were infected, including at least one person who had symptoms. Two died.
Several factors conspired, Ms. Hamner said. When singing, people can emit many large and small respiratory particles. Singers also breathe deeply, increasing the chance they will inhale infectious particles.
Similar transmission dynamics could be at play in other settings where heavy breathing and loud talking are common over extended periods, like gyms, musical or theater performances, conferences, weddings and birthday parties. Of 61 clusters of cases in Japan between Jan. 15 and April 4, many involved heavy breathing in close proximity, such as karaoke parties, cheering at clubs, talking in bars and exercising in gyms, according to a recent study in the journal Emerging Infectious Diseases.
An estimated 10% of people with Covid-19 are responsible for about 80% of transmissions, according to a study published recently in Wellcome Open Research. Some people with the virus may have a higher viral load, or produce more droplets when they breathe or speak, or be in a confined space with many people and bad ventilation when they’re at their most infectious point in their illness, said Jamie Lloyd-Smith, a University of California, Los Angeles professor who studies the ecology of infectious diseases.
But overall, “the risk of a given infected person transmitting to people is pretty low,” said Scott Dowell, a deputy director overseeing the Bill & Melinda Gates Foundation’s Covid-19 response. “For every superspreading event you have a lot of times when nobody gets infected.”
The attack rate for Covid-19 in households ranges between 4.6% and 19.3%, according to several studies. It was higher for spouses, at 27.8%, than for other household members, at 17.3%, in one study in China.

Rosanna Diaz with her son Tomas. PHOTO: ROSANNA DIAZ
Rosanna Diaz lives in a three-bedroom apartment in New York City with five other family members. The 37-year-old stay-at-home mother was hospitalized with a stroke on April 18 that her doctors attributed to Covid-19, and was still coughing when she went home two days later.
She pushed to get home quickly, she said, because her 4-year-old son has autism and needed her. She kept her distance from family members, covered her mouth when coughing and washed her hands frequently. No one else in the apartment has fallen ill, she said. “Nobody went near me when I was sick,” she said.
No one knows for sure how much virus it takes for someone to become infected, but recent studies offer some clues. In one small study published recently in the journal Nature, researchers were unable to culture live coronavirus if a patient’s throat swab or milliliter of sputum contained less than one million copies of viral RNA.
“Based on our experiment, I would assume that something above that number would be required for infectivity,” said Clemens Wendtner, one of the study’s lead authors and head of the department of infectious diseases and tropical medicine at München Klinik Schwabing, a teaching hospital at the Ludwig Maximilian University of Munich.
He and his colleagues found samples from contagious patients with virus levels up to 1,000 times that, which could help explain why the virus is so infectious in the right conditions: It may take much lower levels of virus than what’s found in a sick patient to infect someone else.
Changing policies
Based on this emerging picture of contagion, some policies are changing. The standard procedure for someone who tests positive is to quarantine at home. Some cities are providing free temporary housing and social services where people who are infected can stay on a voluntary basis, to avoid transmitting the virus to family members.
The CDC recently urged Americans to keep wearing masks and maintaining a distance from others as states reopen. “The more closely you interact with others, the longer the interaction lasts, the greater the number of people involved in the interaction, the higher the risk of Covid-19 spread,” said Jay Butler, the CDC’s Covid-19 response incident manager.
If the number of Covid-19 cases starts to rise dramatically as states reopen, “more extensive mitigation efforts such as what were implemented back in March may be needed again,” a decision that would be made locally, he said.
CDC guidelines for employers whose workers are returning include requiring masks, limiting use of public transit and elevators to reduce exposure, and prohibiting hugs, handshakes and fist-bumps. The agency also suggested replacing communal snacks, water coolers and coffee pots with prepacked, single-serve items, and erecting plastic partitions between desks closer than 6 feet apart.

A crowd gathered at a bar in Columbus, Ohio, on May 15. PHOTO: DORAL CHENOWETH/THE COLUMBUS DISPATCH/ASSOCIATED PRESS
Current CDC workplace guidelines don’t talk about distribution of aerosols, or small particles, in a room, said Lisa Brosseau, a respiratory-protection consultant for the University of Minnesota’s Center for Infectious Disease Research and Policy.
“Aerosol transmission is a scary thing,” she said. “That’s an exposure that’s hard to manage and it’s invisible.” Ensuring infected individuals stay home is important, she said, but that can be difficult due to testing constraints. So additional protocols to interrupt spread, like social distancing in workspaces and providing N95 respirators or other personal protective equipment, might be necessary as well, she said.
Some scientists say while aerosol transmission does occur, it doesn’t explain most infections. In addition, the virus doesn’t appear to spread widely through the air.
“If this were transmitted mainly like measles or tuberculosis, where infectious virus lingered in the airspace for a long time, or spread across large airspaces or through air-handling systems, I think you would be seeing a lot more people infected,” said the CDC’s Dr. Brooks.
Sampling the air in high-traffic areas regularly could help employers figure out who needs to get tested, said Donald Milton, professor of environmental and occupational health at the University of Maryland School of Public Health.
“Let’s say you detect the virus during lunchtime on Monday in a dining hall,” he said. “You could then reach out to people who were there during that time telling them that they need to get tested.”
Erin Bromage, a University of Massachusetts Dartmouth associate professor of biology, has been fielding questions from businesses, court systems and even therapists after a blog post he wrote titled “The Risks—Know Them—Avoid Them” went viral.
Courts are trying to figure out how to reconvene safely given that juries normally sit close together, with attorneys speaking to them up close, Dr. Bromage said. Therapists want to be able to hold in-person counseling sessions again. And businesses are trying to figure out what types of cleaning and disease-prevention methods in which to invest most heavily.
He advises that while wiping down surfaces and putting in hand-sanitizer stations in workplaces is good, the bigger risks are close-range face-to-face interactions, and having lots of people in an enclosed space for long periods. High-touch surfaces like doorknobs are a risk, but the virus degrades quickly so other surfaces like cardboard boxes are less worrisome, he said. “Surfaces and cleaning are important, but we shouldn’t be spending half of our budget on it when they may be having only a smaller effect,” he said.

Plexiglass dividers at the Bellagio Hotel and Casino in Las Vegas on June 4. PHOTO: JOE BUGLEWICZ/BLOOMBERG NEWS
Drugmaker Eli Lilly & Co. has a medical advisory panel that’s reading the latest literature on viral transmission, which it is using to develop recommendations for bringing back the company’s own workers safely.
To go into production facilities, some of which are in operation now, scientists must don multiple layers of personal protective equipment, including gloves, masks, goggles and coveralls. That’s not abnormal for drug-development settings, said Lilly Chief Scientific Officer Daniel Skovronsky. “The air is extensively filtered. There’s lots of protection,” he said.
The places he worries about are the break rooms, locker rooms and security checkpoints, where people interact. Those are spaces where the company has instituted social-distancing measures by staggering the times they are open and how many people can be there at once. Only a few cafeterias are open, and those that are have socially distanced seating. In bathrooms, only half the stalls are available to cut down on the number of people.
“We’ll never be more open than state guidelines,” Dr. Skovronsky said, but “we’re often finding ourselves being more restrictive because we’re following the numbers.”